We have taken a novel approach, developing a real-time, accurate, and non-invasive technology to monitor free flap viability at the bedside. This project is leading by Dr. Donald Anderson and Dr. Babak Shadgan.
Free tissue transfer (FFT) is a surgical procedure for reconstructing composite hard & soft tissue defects after severe injuries or following cancer surgeries where a significant portion of the body is lost or must be removed. Free tissue transfer involves harvesting a portion of vital tissue from one area of the body, e.g., leg, arm, or torso, and transferring it to reconstruct and fill in a defect in another area, e.g. wound in the mouth or face. This procedure requires vigilant postoperative monitoring and care. Within 72 hours after surgery, flap viability is at risk of compromise. Obstruction of anastomosed vessels due to compression, clot, emboli, or torsion occurs in 5 to 25% of cases. When free flap failure is recognized, the patient must be immediately re-operated for an attempted salvage of the microvascular anastomosis. In the event of flap death, due to delayed or unsuccessful salvage, the patient must undergo multiple surgeries that compound the morbidity, prolong the hospital stay, increases health care costs and impairs quality of life. Early detection of vascular compromise is, therefore, essential for increasing the odds of successful salvage. The current standard for postoperative monitoring of free flap viability is based on clinical examination, which is time-consuming, subjective, delayed, and prone to error. Furthermore, buried flaps, like those in the oral cavity, cannot be directly visualized and examined.
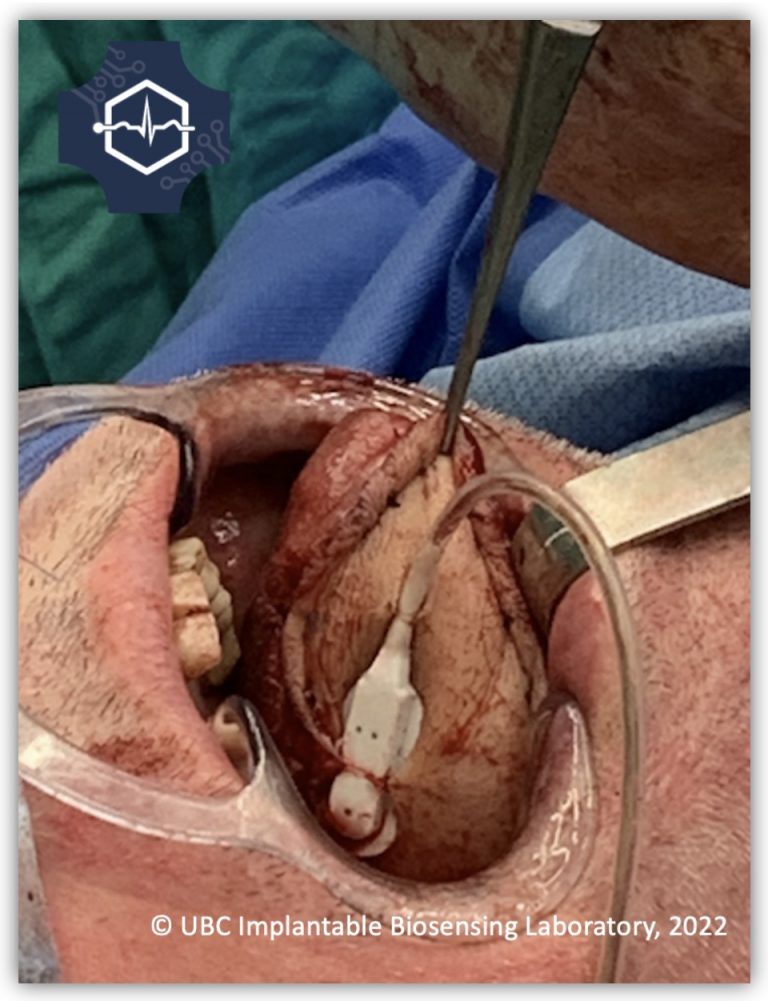
We apply a novel configuration of NIRS technology to monitor free flap tissue oxygenation, perfusion, and vital signs. Using our implantable and miniaturized NIRS sensor, we monitor the tissue oxygen saturation level of free flaps transplanted at any part of the body. This critical information will improve surgical outcomes and flap survival rates by earlier and more precise detection of vascular compromise. On the health care delivery level, eventual reliance on optical monitoring of free flaps can decrease the chance of multiple surgeries and overall surgical morbidity, shorten postoperative hospitalization and reduce associated costs. The novel intervention we are developing has the propensity to improve reconstructive surgery and wound healing in Canada and worldwide.
Related Publications
- Newton E, et al., (2019); DOI: 10.1002/micr.30526
Supported By:

